Introduction: Patients with sickle cell disease (SCD) develop acute episodes of pain for which they seek care in the hospital emergency department (ED). Infusion center (IC)-based care is an effective alternate treatment strategy for management of uncomplicated pain episodes. However, at our center, we could not obtain institutional buy in for dedicated IC resources. Hence, we developed a telemedicine-guided “add on” IC model, embedded within our institution's cancer infusion services. Here, we evaluate the feasibility of our telemedicine-guided IC model and its effectiveness in managing acute pain episodes and impact on SCD patient care.
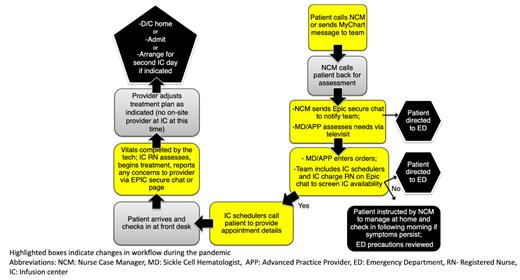
Methods: A multi-disciplinary team consisting of the SCD clinical team including Nurse Case Manager, Advanced Practice Provider (APP), MD and the IC team including IC leadership, IC charge RN, IC scheduler was assembled. An agreement was made between the SCD team and IC leadership that at least one “add on slot” would be made available for an acute SCD pain visit every day. A workflow was created integrating telemedicine for communication with patients and team members alike, and all team members were educated regarding the workflow (Figure 1). IC leadership was re-engaged when changes needed to be made to the workflow to accommodate more IC visits. Visit numbers for IC visits, emergency department (ED) same day discharges and inpatient (IP) hospitalizations were collected from the electronic medical record and compared for pre-IC development (Jan 1, 2017- Dec 31, 2018) and post IC (January 1, 2021 - Dec 31, 2022). Statistical analysis was performed using Graphpad/Prism assuming nonparametric distribution where applicable.
Results: We were able to successfully implement our telemedicine-based IC workflow for management of acute SCD pain. Given the rapid increase in IC requests and need for accommodating more than one patient a day, we engaged nursing leadership and re-designed the workflow to identify additional “add on” slots at various IC locations in our health system, added extended hours and weekend capacity. IC visits for uncomplicated pain episodes increased nearly 9 fold, from 132 visits in the pre-IC period to 1151 visits in the post IC period. Seventeen patients used the IC in the pre-telemedicine period and 53 patients used the IC in the post-telemedicine period. The number of ED same day discharges decreased by 35.2%, from 372 visits in pre-IC phase to 241 visits in post IC period. The number of IP hospitalizations went from 281 to 278. ED visits per IC user per year decreased from 10.9 to 2.4 and IP hospitalizations per IC user per year decreased from 8.3 to 2.6.
There was a positive correlation between number of IC visits and ED discharges (Spearman r 0.27, p= 0.06) and between number of IC visits and inpatient hospitalizations (Spearman r 0.4, p=0.006), indicating that the patients who were high users of IC based services also had high rates of ED use and hospitalizations. Twenty four patients who used the IC in 2022 did not have same day ED discharges, 15 patients did not have IP stays and 10 patients did not have IP or ED visits in 2022. Among these 10 patients, 8 had their first IC contact under the telemedicine triage IC model (2021-2022).
Conclusions: Telemedicine based IC triage can be a successful model for delivery of IC based care for management of acute SCD pain and of great value in settings where dedicated resources are not available. The total number of ED discharges decreased after incorporation of our model, as did both ED discharges and IP hospitalizations per IC user per year. Patients with high numbers of IC visits were also high utilizers of hospital-based services. A cohort of patients were able to use the IC alone for pain management and did not use the ED or get hospitalized.
Disclosures
Gopal:Alexion: Speakers Bureau; bluebird bio: Honoraria.